Blue Cross and Blue Shield of North Carolina (Blue Cross NC) is expanding the Blue High Performance NetworkSM (BlueHPNSM).
BlueHPN is a national quality-based network that provides members with access to high-quality doctors, hospitals and specialists across the state and country - all while lowering costs. Over 185 million Americans now have access to BlueHPN nationally.
Blue Cross NC is collaborating with participants of Blue Premier with Blue HPN to hold both us and health systems accountable for better health outcomes, exceptional experiences and lower costs.
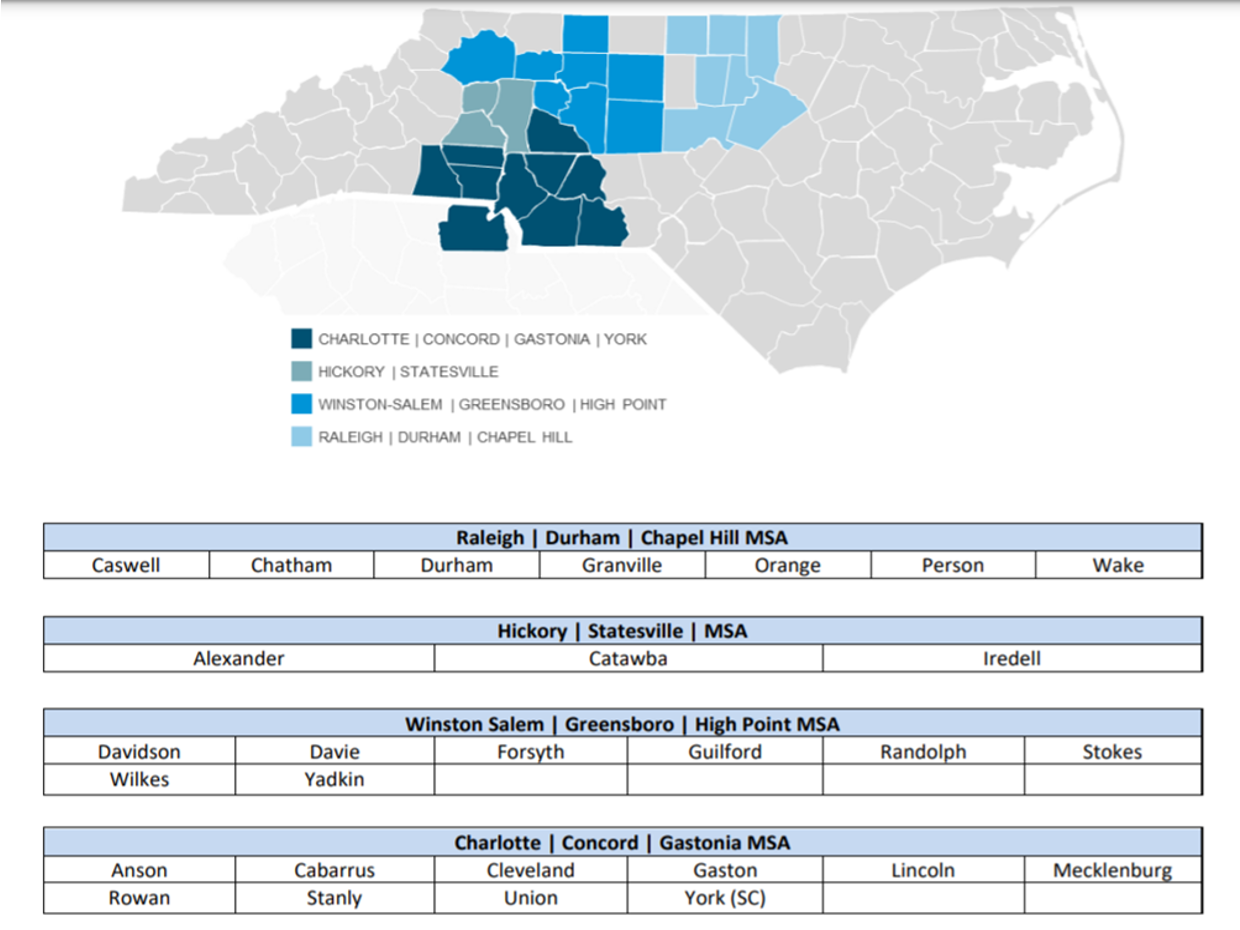
BlueHPN providers are available in:
- Triad area: Atrium Health Wake Forest Baptist (formerly Wake Forest Baptist Health)
- Charlotte area: Atrium Health
- Triangle area: Duke Health/Aledade
- Hickory area: Frye Regional Medical Center, Iredell Memorial Medical Center, Aledade and Community Care Physician Network (CCPN)
BlueHPN will expand to other areas of the state beyond January 2022.
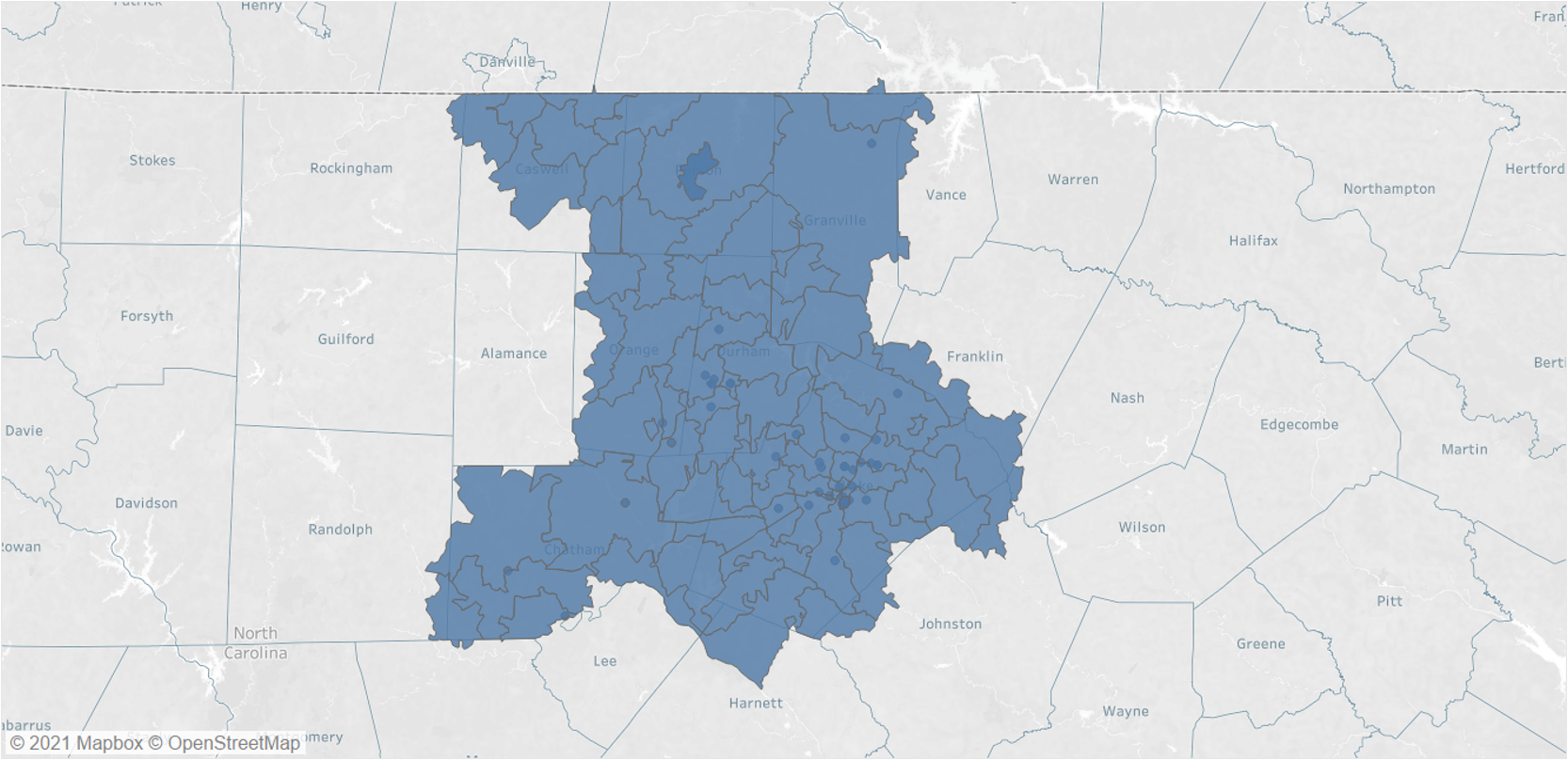
BlueHPN Service Areas
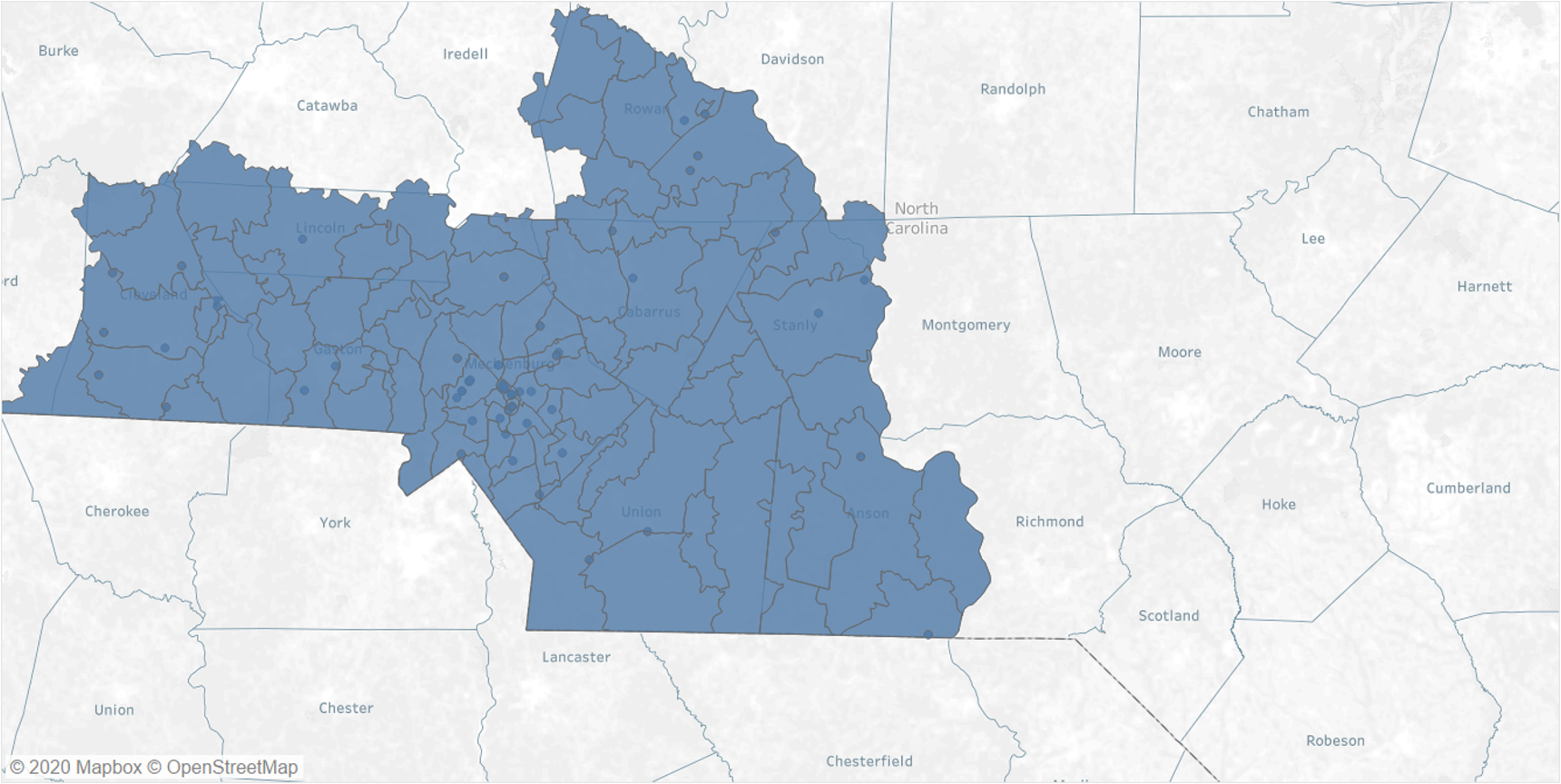
Charlotte Area
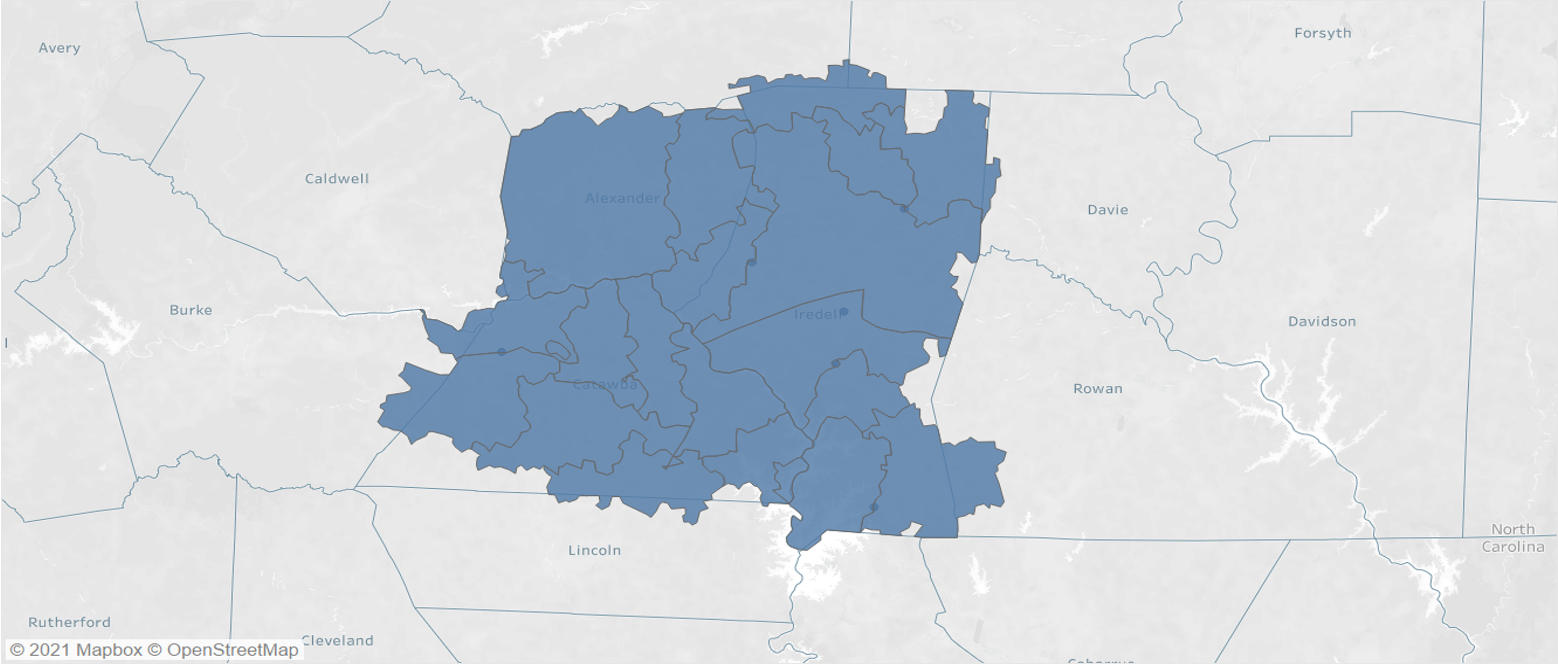
Hickory Area
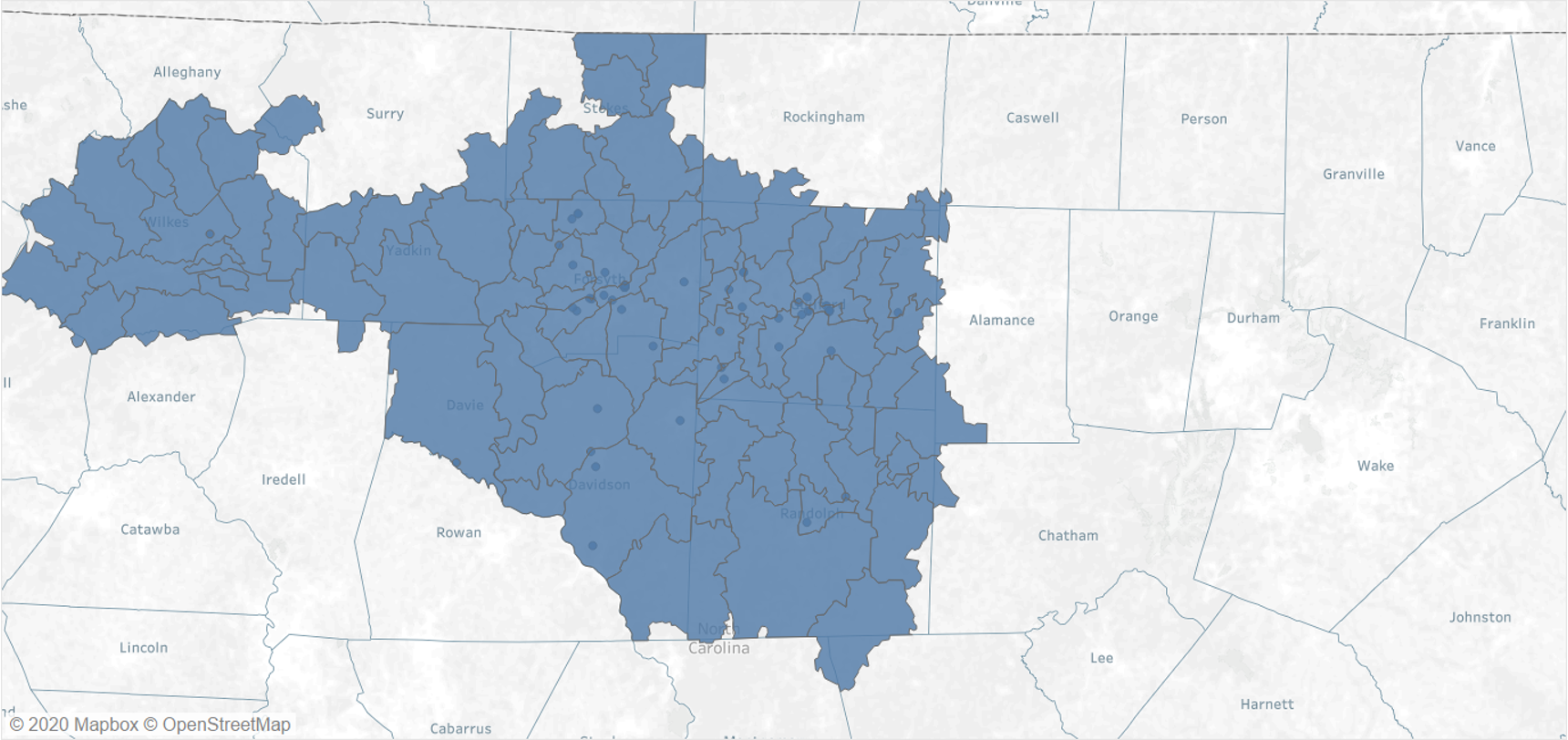
Triad Area
Triangle Area
BlueHPN Frequently Asked Questions
Blue Cross and Blue Shield of North Carolina (Blue Cross NC) contracts with health care providers to be in BlueHPN. Your office manager or contracting manager/representative will have information on the networks you participate in, including BlueHPN.
As a BlueHPN health care provider, your practice will appear on our online “Find a Doctor” tool when a provider search is done in your geographic area. If you would like to confirm this, we can instruct you on how to conduct a search using the “Find a Doctor” tool., or please reference the instructions below. Please contact the Provider Blue Line at 800-214-4844 if you need additional assistance.
- Click the link Find a Doctor from any page on BlueCrossNC.com.
- Select one of the following options to initiate the provider search.
- Individuals, Families & Groups
- Dental
- Medicare
- Choose the Blue High Performance Network plan from the drop-down box options.
- Once the plan has been selected, determine the appropriate tile for your search – Provider, Facility for Medical Care, Dental Care, or Urgent Care – and select the appropriate tile accordingly.
- The next screen will show a Browse by Category button, as well as a Search field.
- Click the Browse by Category button to reveal a clickable menu, or you also have the option of a keyword search in the Search field.
- If using the search field, type your practice or provider name in the search field. Once the name is typed, press enter or select the provider if auto-populated.
- Once you have selected your practice or provider name that meets your search, click on the provider name to find more details on the profile, and verify BlueHPN par status under the plans accepted section. If not using the search field, the steps below outline directions to browse by Medical Speciality.
- Click the appropriate item that suits your practice (e.g., Medical Specialties).
- Click the appropriate medical specialty (e.g., Specialist).
- Click the appropriate specialist category (e.g., Dermatology). Each item represents a group of certain types of providers.
- Select the item that appropriately suits your needs. A listing of the selected specialists appears. This list can span multiple pages.
- Once you have selected the type of provider that fits your search, click on the provider to find more details on their profiles, and verify BlueHPN par status under the plans accepted section.
If your practice is a BlueHPN Provider, all providers under the practice are considered participating under the BlueHPN product. Please contact your office manager or contracting manager/representative. You may also use our “Find a Doctor” tool or contact the Provider Blue Line at 800-214-4844.
If you are a Blue Distinction Specialty Care (BDSC) or Total Care designated healthcare provider and have a signed agreement to participate in BlueHPN, you are considered a BDSC and/or Total Care Designated Health Care provider. Please contact the Provider Blue Line at 800-214-4844 if you have any further questions.
This will depend upon whether BlueHPN patients are included in the value-based contract you or your organization has with Blue Cross NC. Please contact your Blue Cross NC contracting representative to confirm.
Please contact the Provider Blue Line at 800-214-4844 to ensure that we have all the information needed from you for an accurate display on the online “Find a Doctor” tool.
At this time, BlueHPN is only offered to Administrative Services Only (ASO), Self-Funded commercial employer groups.
Eligibility, Benefits and Claim Submission Procedures
BlueHPN patients can easily be identified by looking at their Blue Cross NC member ID card. The Blue High Performance Network name will be prominently displayed on the front of the member ID card, along with the “BlueHPN in a suitcase” logo. This “BlueHPN in a suitcase” logo indicates that PPO rates apply unless your provider contract indicates otherwise. If you don’t see the Blue High Performance Network name or the “BlueHPN in a suitcase” logo on the front of the member ID card, then the patient is not in BlueHPN.
In general, the same procedures apply for both BlueHPN and BlueCard PPO patients. For example, you will check eligibility and benefits, conduct pre-service review, and submit claims using the same contacts and procedures as you do today. One thing to keep in mind, BlueHPN members have limited out of network benefits. Please see the illustration below that provides clarification regarding BlueHPN members In and Out of network benefits.
Medical Benefit |
Place of Service |
Covered Services |
| Participating BlueHPN Provider | ||
|
Preventive Care Routine Care Urgent Care Emergency Care |
Inside BlueHPN Svc Area | Yes |
| Non-Participating BlueHPN Provider | ||
| Emergency Care | Inside BlueHPN Svc Area | Yes |
|
Preventive Care Routine Care Urgent Care |
Inside BlueHPN Svc Area | No |
| Urgent Care/Emergency Care | Outside BlueHPN Svc Areas | Yes |
|
Preventive Care Routine Care |
Outside BlueHPN Svc Areas | No |
It is essential to identify specialists that are in BlueHPN using the “Find a Doctor” tool before making a recommendation to your patient. This is meant to avoid having your patient pay unexpected out-of-pocket costs. If you cannot find an appropriate specialist within BlueHPN to treat your patient's condition, contact the Provider Blue Line at 800-214-4844 as there are exceptions to make sure your BlueHPN patients get the care they need. This is always our priority.
Please contact Blue Cross NC by using the Provider Blue Line at 800-214-4844. There are exceptions to make sure your BlueHPN patients get the care they need. Naturally, our priority is the health of our members.
Non-Participating Health Care Providers
BlueHPN is currently closed to network additions. When the anchoring health systems and Blue Cross NC developed these networks, we did an intensive analysis of network adequacy, accessibility, and marketability, incorporating both CMS and NCDOI guidelines. We review network adequacy for each product annually. If you have further questions or concerns, please call Provider Blue Line at 800-214-4844.
Quality Measurement
We believe greater value can be achieved by working with healthcare providers to elevate the level of care delivered to patients. A “one-size-fits-all” application of a quality threshold does not account for variation in local healthcare dynamics, appropriateness, and evolving population health priorities. Quality performance requirements for local healthcare provider participation in BlueHPN are determined by evaluating against local, regional, state and/or national benchmarks. Our efforts in this area will continue to evolve.
When selecting national measures for BlueHPN, we identified measures that:
- Are aligned with industry-recognized standards, such as the Catalyst for Payment Reform
- Are most commonly used to establish healthcare provider accountability for better patient outcomes
- Closed clinical care gaps, impact longevity and quality of life and/or lower costs
- Spanned care settings and provider types (primary care, specialists and hospitals) to provide a more holistic view of clinical quality performance
- Accounted for regulatory and/or state mandates
- Created a foundation and framework for continuous improvement
We select quality measures that address key healthcare challenges in each local market, prioritizing measures that align with community health disparities, or those that incentivize better performance in areas that address local needs or challenges. For example, diabetes management might be a critical quality indicator in one community while improving immunization adherence is higher priority in another.
The measures that organizations will be measured on are below. They include both national measures and Blue Cross NC locally selected measures.
Quality Category |
National Quality Core Measure |
National Quality Data Score |
NC Quality Local Measure |
Blue Cross NC Local Quality Measure |
|---|---|---|---|---|
|
1. Appropriate Care: Reduces healthcare waste and prevents patient harm |
Asthma Medication Ratio | NCQA HEDIS | Medication Management in People with Asthma (75%) | NCQA HEDIS |
| Use of Imaging Studies for Low Back Pain | NCQA HEDIS | Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis | NCQA HEDIS | |
|
2. Best Practice Adherence: Uses evidence-based medicine |
Elective delivery | CMS Hospital Compare (Care Compare) | Controlling High Blood Pressure | NCQA HEDIS |
| Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment | NCQA HEDIS | Pharmacotherapy Management COPD Exacerbation (PCE)- Bronchodilator | NCQA HEDIS | |
|
3. Better Health Management: Focuses on preventing illness and better managing chronic conditions |
Breast Cancer Screening | NCQA HEDIS | Child and Adolescent Well- Care Visits (AWC) | NCQA HEDIS |
| Statin Therapy for Patients with Cardiovascular Disease | NCQA HEDIS | Colorectal Cancer Screening | NCQA HEDIS | |
|
4. Improved Outcomes: To improve the effectiveness of care delivered |
Hospital-Wide All-Cause Unplanned Readmission Measure | CMS Hospital Compare (Care Compare) | Persistence of Beta-Blocker Treatment after a Heart Attack | NCQA HEDIS |
| Methicillin-resistant Staphylococcus Aureus (MRSA) Blood Infections | CMS Hospital Compare (Care Compare) | National Healthcare Safety Network (NHSN): Clostridium difficile | CMS Hospital Compare (Care Compare) |
Processes are already in place to collect and submit Healthcare Effectiveness Data and Information Set (HEDIS) and Hospital Compare quality measure data, which is some of the information we assess to measure quality. National quality measures from the National Committee for Quality Assurance (NCQA), HEDIS and the Centers for Medicare and Medicaid Services (CMS) Hospital Compare were primarily used. There is no current need for additional data to be submitted to plans at this time.
HEDIS is one of the most widely used set of healthcare performance measures in the United States. HEDIS includes 95 measures across seven domains of care. NCQA has expanded the size and scope of HEDIS to include measures for physicians, PPOs and other organizations.
Hospital Compare (Care Compare), on the other hand, was created through the efforts of CMS and has information about the quality of care at over 4,000 Medicare-certified hospitals across the country. The information on Hospital Compare helps patients make decisions about where to get their healthcare and encourages hospitals to improve the quality of care they provide.
BlueHPN healthcare providers are measured individually and at an aggregate network level. Quality is measured across all aspects of care delivery (e.g., inpatient, outpatient) and within each provider type (e.g., primary care, specialist, hospital or health system). This approach was established because:
- Individual performance results allow us to identify opportunities for improvement and to recognize higher value care
- Aggregating quality results allows us to understand BlueHPN market level performance in comparison to our BlueCard PPO healthcare provider population
In the near future, score cards will be created and discussed with providers.
We deliberately designed BlueHPN to evolve over time so it will reflect behavior change and account for improved healthcare provider performance to focus more on outcomes measures. As we evaluate the performance of BlueHPN healthcare providers, our selection criteria and measurement approach will be refined to ensure the network continues to improve. We’re committed to working with you to continue influencing care quality and affordability. Our data sharing philosophy and collaborative partnerships gives providers, like you, the insight they need to understand the path toward improvement.


 Blue Connect
Blue Connect